Imagine this: you’re sitting at your desk, working away, when suddenly, a sharp, stabbing pain erupts in your lower abdomen. It feels like a muscle is cramping, but it’s deeper, more intense, and it won’t seem to let go. You try to stretch, you shift positions, you even try to breathe deeply, but the pain persists, leaving you feeling helpless and frustrated. This, my friends, is the dreaded pelvic floor spasm, a condition that affects countless individuals, causing discomfort and disrupting their daily lives.
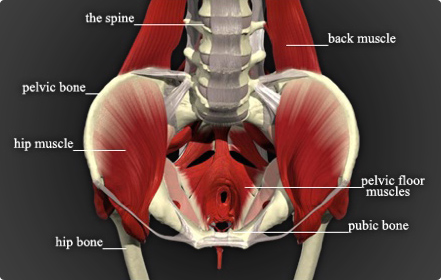
Image: sedonaphysicaltherapy.com
It’s a common misconception that pelvic floor spasms are solely a ‘women’s issue.’ While it’s true that women are more likely to experience them, men are not immune. Regardless of your gender, understanding this condition is crucial for addressing the pain and restoring your quality of life. Let’s dive into the fascinating, yet often uncomfortable, world of pelvic floor spasms to gain a deeper understanding of this prevalent issue.
What is a Pelvic Floor Spasm?
The pelvic floor is a group of muscles that acts like a hammock supporting your organs in your lower abdomen, including your bladder, uterus (women), prostate (men), and rectum. When these muscles contract involuntarily and persistently, it’s considered a pelvic floor spasm. Imagine a muscle in your leg suddenly and unexpectedly tightening without your control, and that’s essentially what it feels like in your pelvic floor.
Pelvic floor spasms can vary in intensity and duration. Some individuals experience a fleeting, sharp pain, while others endure chronic, debilitating discomfort. The pain can be felt in different areas, including the lower abdomen, back, and even the legs. The discomfort can range from a dull ache to intense cramping, and may be accompanied by other symptoms, such as urinary frequency, constipation, and pain during intercourse.
Unveiling the Causes of Pelvic Floor Spasms
Understanding the causes behind pelvic floor spasms is key to finding the right treatment. While the exact reason behind these spasms can vary, we know that various factors can contribute to their development:
Common Causes:
- Prolonged sitting: Spending long hours sitting at work or on long car rides can put undue pressure on the pelvic floor muscles, leading to tension and spasms.
- Stress and anxiety: When we’re stressed, our bodies naturally tense up, and this often includes the pelvic floor muscles. This can lead to chronic muscle tightness and eventually spasms.
- Trauma: Trauma, such as childbirth, surgery, or pelvic floor injury, can lead to inflammation and muscle dysfunction, subsequently triggering spasms.
- Constipation: Straining during bowel movements can put immense pressure on the pelvic floor muscles, increasing their susceptibility to spasms.
- Chronic pain conditions: Certain conditions like endometriosis, fibroids, and irritable bowel syndrome (IBS) can cause pelvic pain and contribute to the development of spasms.
- Lifestyle factors: Certain habits like smoking, excessive alcohol consumption, and caffeine intake can worsen pelvic floor spasm symptoms.

Image: zakruti.com
Decoding the Symptoms of Pelvic Floor Spasm
Identifying the subtle signs of pelvic floor spasm is crucial for seeking timely medical attention. While pain is the most common symptom, other indicators may also emerge, including:
A Spectrum of Symptoms:
- Pain: A sharp, stabbing pain that may come and go, or a persistent dull ache in the lower abdomen, back, or pelvic area.
- Urinary Issues: Frequent urination, difficulty starting urination, or a feeling of incomplete bladder emptying.
- Bowel Issues: Constipation, pain during bowel movements, or a feeling of incomplete bowel evacuation.
- Pain during intercourse: Discomfort or pain during sexual activity, often accompanied by a feeling of tightness or muscle tension.
- Low back pain: The pain may radiate from the pelvic region to the lower back.
- Pain with certain movements: Discomfort with activities like stretching, yoga, or exercises that involve the pelvic floor muscles.
Seeking Medical Guidance: Identifying and Diagnosing Pelvic Floor Spasms
If you’re experiencing any of the symptoms mentioned above, consulting a healthcare professional is essential. A comprehensive diagnosis can help you understand the root of your discomfort and receive the appropriate treatment.
Your healthcare provider will likely begin by taking a detailed medical history, reviewing your symptoms, and conducting a physical examination. They may also perform some additional tests to rule out other conditions, such as:
- Pelvic floor muscle assessment: This involves examining the strength and flexibility of your pelvic floor muscles to identify any imbalances or dysfunctions.
- Ultrasound: This imaging technique can help visualize the pelvic floor muscles and identify any abnormalities.
- Urinary studies: These tests may include uroflowmetry (measuring urine flow rate) and post-void residual volume (measuring urine left in the bladder after urination) to evaluate bladder function.
- Rectal examination: This involves examining the rectum to assess the tone and function of the pelvic floor muscles.
Navigating the Treatment Landscape: Relieving Pelvic Floor Spasms
Once your condition is diagnosed, your healthcare provider will work with you to develop a personalized treatment plan. The goal is to address the underlying cause of your spasms and reduce your symptoms. Treatment options may include:
Common Treatments:
- Pelvic floor muscle relaxation techniques: This involves learning to identify and release tension in your pelvic floor muscles through various techniques, such as deep breathing exercises, biofeedback, or massage.
- Physical therapy: A pelvic floor physical therapist can provide specialized exercises and manual therapy techniques to strengthen and stretch the pelvic floor muscles, restoring their optimal function.
- Medications: In some cases, your doctor may prescribe medications, such as muscle relaxants or anti-inflammatory drugs, to help reduce pain and discomfort.
- Lifestyle changes: Modifying your diet, reducing stress levels, avoiding alcohol and caffeine, and maintaining a healthy weight can all contribute to relieving symptoms and improving your overall well-being.
- Botox injections: In more severe cases, Botox injections into the pelvic floor muscles may be considered to temporarily block nerve signals and reduce muscle spasms.
Empowering Yourself: Tips and Expert Advice
Living with pelvic floor spasms can be challenging, but there are steps you can take to manage your condition and improve your daily life:
Your Toolkit for Relief:
- Practice relaxation techniques: Regular stress management techniques, such as mindfulness meditation, yoga, or deep breathing exercises, can be beneficial in reducing muscle tension and promoting overall well-being.
- Maintain a healthy lifestyle: A balanced diet, regular exercise, adequate sleep, and limiting caffeine and alcohol can all contribute to symptom management and overall health.
- Seek support from a therapist: Talking to a therapist can provide emotional support and help you develop coping mechanisms for dealing with the emotional toll of chronic pain.
- Join a support group: Connecting with others who understand your condition can provide valuable insights, encouragement, and a sense of community.
It’s essential to remember that you’re not alone in this journey. There are numerous resources available to help you navigate the challenges of pelvic floor spasms. With the right support and treatment, you can regain control over your body and find relief from this often misunderstood condition.
Frequently Asked Questions (FAQ)
Q: What are some causes of pelvic floor spasms?
A: Pelvic floor spasms can be caused by a variety of factors, including prolonged sitting, stress and anxiety, trauma, constipation, chronic pain conditions, and certain lifestyle choices like smoking and alcohol consumption.
Q: Is pelvic floor spasm a common condition?
A: While it’s not always openly discussed, pelvic floor spasms are surprisingly common, affecting a significant number of individuals. Many people, especially women, experience these symptoms but may not realize it’s a treatable condition.
Q: Can a pelvic floor physical therapist help with spasms?
A: Absolutely! Pelvic floor physical therapists are specifically trained to work with these muscles, providing targeted exercises and manual therapy techniques to strengthen, stretch, and re-educate the pelvic floor muscles, leading to symptom relief and improved function.
Q: What if medication doesn’t work for my pelvic floor spasms?
A: If medication alone isn’t effective, your healthcare provider may recommend alternative or combined treatment approaches, such as physical therapy, relaxation techniques, lifestyle modifications, and even Botox injections in more severe cases.
Q: Can I prevent pelvic floor spasms?
A: While you can’t always prevent spasms, adopting healthy habits can significantly reduce your risk. This includes maintaining a healthy weight, managing stress, avoiding excessive sitting, and making sure you’re not constipated.
What Does A Pelvic Floor Spasm Feel Like
https://youtube.com/watch?v=jft2xF5NERs
Conclusion
Pelvic floor spasms can be a confusing and painful experience, but with awareness and the right treatment, you can find relief. Remember that this condition is treatable, and there are resources available to support you. If you are experiencing any pelvic pain or discomfort, please don’t hesitate to consult a healthcare professional, and be sure to ask about pelvic floor physical therapy. Remember, you are not alone, and there is hope for a brighter, pain-free future.
Are you interested in learning more about pelvic floor spasms and how to manage them? Let us know in the comments below, and we’re happy to share more information and resources with you!



/GettyImages-173599369-58ad68f83df78c345b829dfc.jpg?w=740&resize=740,414&ssl=1)


