Imagine waking up one morning with a sharp, searing pain in your lower back. You’re unable to stand straight, let alone bend over to pick up a dropped pen. The pain radiates down your leg, a constant, throbbing reminder of something very wrong. This, unfortunately, is a reality for many people living with a broad-based disc protrusion. It’s a condition that often goes unnoticed until the pain becomes unbearable, leaving many feeling frustrated, confused, and desperate for relief.
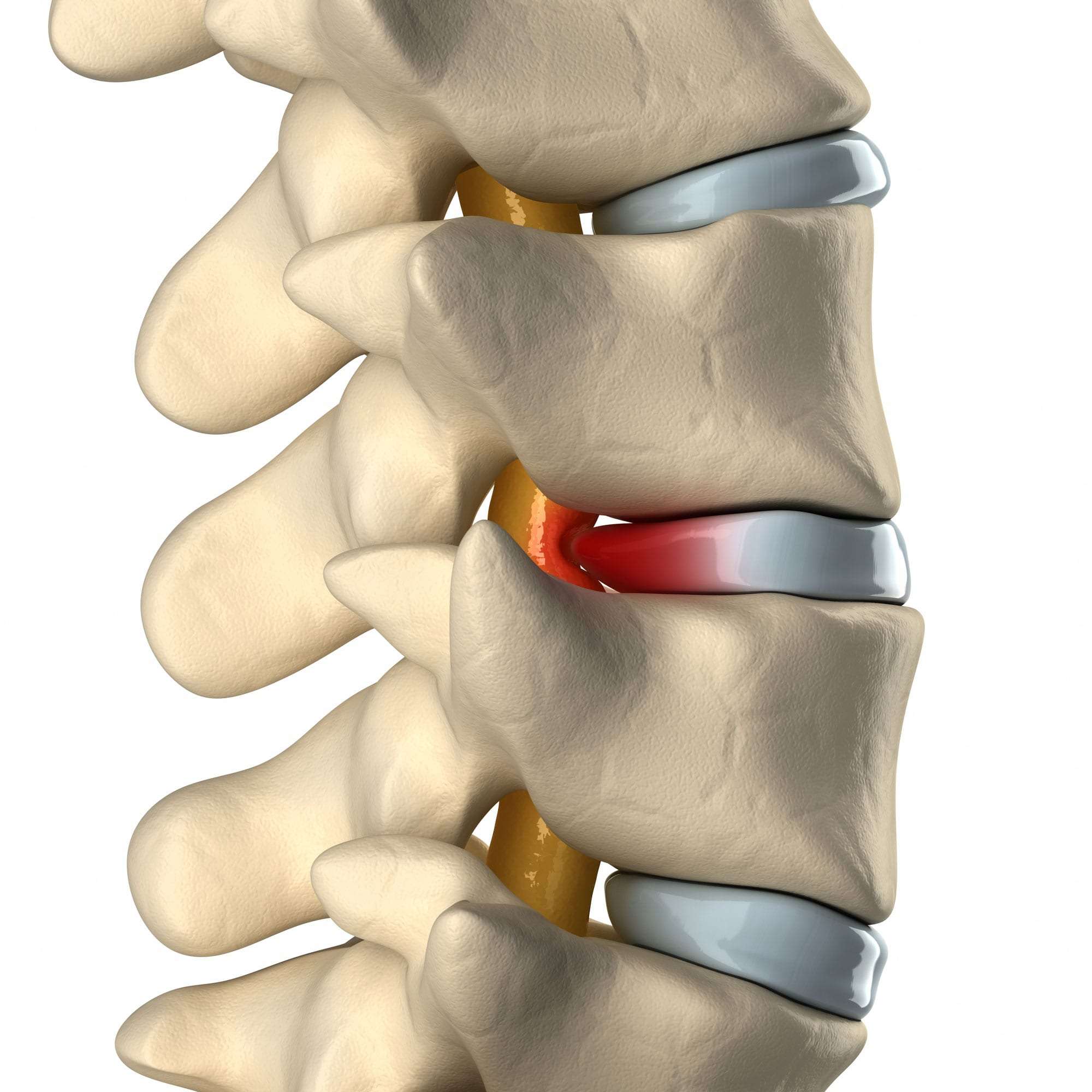
Image: novusspinecenter.com
But what exactly is a broad-based disc protrusion? And how can you understand this silent sufferer that is taking over your life? This article dives into the intricacies of this condition, helping you understand the cause, symptoms, diagnosis, and treatment options. By shedding light on this often-overlooked condition, we aim to empower you with the knowledge to navigate this challenging experience.
A Deep Dive into Broad-Based Disc Protrusion: Unveiling the Silent Sufferer
Our spine is a complex structure, designed to support our body and allow for movement. At the center of each spinal vertebra lies an intervertebral disc, a shock absorber made of a tough outer layer (annulus fibrosus) and a soft, gel-like center (nucleus pulposus). When these discs experience a tear or rupture, the inner gel-like material leaks out, pushing against the surrounding nerves. This bulging disc, known as a disc protrusion, can cause pain and other symptoms depending on its location and severity.
Specifically, a broad-based disc protrusion refers to a bulging disc that protrudes outwards in a wide, flat manner, rather than a localized bulge. This wider protrusion can affect a larger area of nerve roots, potentially leading to more widespread pain and neurological issues.
The Causes Behind the Silent Sufferer:
This condition isn’t a result of a single cause; it often arises from a combination of factors, including:
- Age: As we age, the discs in our spine naturally lose their hydration and elasticity, becoming more susceptible to tears and protrusions.
- Lifestyle: Repetitive heavy lifting, poor posture, and lack of physical activity can place excessive stress on the spine, increasing the risk of disc damage.
- Genetics: Predisposition to disc degeneration can also be inherited.
- Trauma: Accidents or injuries such as a fall or car accident can lead to disc protrusion, sometimes even causing a herniated disc.
Understanding the Silent Sufferer’s Symptoms:
The symptoms of a broad-based disc protrusion can vary depending on the location of the disc protrusion, the severity of the protrusion, and the individual’s overall health. Common symptoms may include:
- Back Pain: Localized pain in the back, often radiating down the legs or arms.
- Sciatica: Sharp, shooting pain that travels down the leg, usually caused by a disc protrusion in the lower back.
- Numbness and Tingling: Loss of sensation in the affected area, often accompanied by weakness.
- Muscle Weakness: Difficulty walking, lifting, or performing daily activities due to muscle weakness.
- Bowel and Bladder Dysfunction: In severe cases, a broad-based disc protrusion can affect the nerves controlling bowel and bladder function, leading to incontinence.

Image: www.medicalexhibits.com
Diagnosis: Unmasking the Silent Sufferer:
Diagnosing a broad-based disc protrusion typically involves a combination of medical history, physical examination, and imaging tests:
- Physical Examination: Your doctor will assess your range of motion, muscle strength, reflexes, and sensory function.
- Imaging Tests:
- X-rays: Can rule out other conditions and help visualize the spine’s alignment.
- Magnetic Resonance Imaging (MRI): Provides detailed images of the spinal cord, discs, and surrounding nerves, offering the best visualization of a disc protrusion.
- Computed Tomography (CT) Scan: Can also help identify the location and extent of the disc protrusion, especially when combined with a myelogram.
Treatment Options for the Silent Sufferer:
Treatment for a broad-based disc protrusion aims to reduce pain, improve function, and prevent further damage.
Non-Surgical Treatment Options:
- Rest and Activity Modification: Avoiding activities that aggravate pain can help your disc heal.
- Pain Medication: Over-the-counter pain relievers like ibuprofen or naproxen, prescription medications, such as opioids or muscle relaxers, can help manage pain.
- Physical Therapy: Physical therapy exercises, stretches, and postural corrections can strengthen muscles, improve flexibility, and reduce pain.
- Epidural Steroid Injections: Steroids can be injected into the epidural space to reduce inflammation and pain.
Surgical Treatment Options:
- Surgery: If conservative treatment fails to provide relief or if neurological function deteriorates, surgery might be recommended. Surgery might involve removing part of the disc or fusing the vertebrae.
Expert Insights and Actionable Tips:
Dr. Emily Evans, a board-certified neurosurgeon, emphasizes the importance of early intervention: “While many people with a broad-based disc protrusion can find relief through conservative treatment, early diagnosis and management are crucial to prevent further complications. If you experience persistent pain or neurological symptoms, don’t hesitate to seek medical attention.”
Here are some actionable tips to manage your broad-based disc protrusion:
- Maintain a Healthy Weight: Excess weight puts extra pressure on your spine.
- Practice Good Posture: Sitting and standing with proper posture can reduce strain on your back.
- Regular Exercise: Strengthening your core muscles can provide better support for your spine.
Broad-Based Disc Protrusion
Conclusion: Empowering You to Take Charge
A broad-based disc protrusion can be a challenging experience, but understanding the condition and its treatment options empowers you to actively manage your pain and improve your quality of life. Remember, seek professional medical advice and don’t hesitate to ask questions. By taking a proactive approach, you can gain control over your health and live a fulfilling life.



/GettyImages-173599369-58ad68f83df78c345b829dfc.jpg?w=740&resize=740,414&ssl=1)


