Imagine a world where your deepest fears, your most intimate struggles, are dissected and displayed in a macabre museum. Where the anguish of mental illness becomes a spectacle for public consumption. This chilling scenario, though fictional, reflects the unease that many feel about the field of psychiatry. It’s a field that, despite its noble intentions to alleviate suffering, has a long and complex history, one often intertwined with controversy, ethical dilemmas, and the question: is psychiatry truly helping, or merely perpetuating the very suffering it claims to cure?

Image: www.cchrflorida.org
This article delves into the heart of this complex issue, exploring the often-overlooked criticisms surrounding psychiatry, challenging the status quo, and ultimately, seeking to empower individuals who are seeking alternative paths to mental wellbeing. Our aim is not to demonize psychiatry, but to shine light on the complexities, the risks, and the potential alternative approaches that are often overlooked.
The Origins of Modern Psychiatry
The roots of modern psychiatry are entangled with a history fraught with both ambition and error. Early practitioners like Emil Kraepelin attempted to classify mental illnesses into distinct categories, laying the groundwork for the Diagnostic and Statistical Manual of Mental Disorders (DSM), the bible of the psychiatric world. The DSM, despite its intent to provide a standardized framework for diagnosis, has been critiqued for its tendency to pathologize everyday human experiences and its potential to medicalize normal emotions.
The Rise of the Pharmaceutical Industry
The 20th century witnessed a dramatic shift in how mental illness was treated, with the advent of psychotropic medications. Antidepressants, anti-anxiety medications, and antipsychotics became the cornerstone of many psychiatric interventions. While these medications offer a lifeline for some, they are not without their downsides. Side effects, including weight gain, insomnia, sexual dysfunction, and even suicidal thoughts, are common. Furthermore, the focus on medication has led some to question whether other forms of therapy, such as talk therapy or holistic approaches, are being neglected.
The Power of the Medical Model
Psychiatry operates under a medical model framework, framing mental illness as a disease residing within an individual’s brain. This model has been instrumental in developing treatments, but it has also been criticized for ignoring the influence of social and environmental factors – poverty, trauma, discrimination – that can significantly impact mental health.
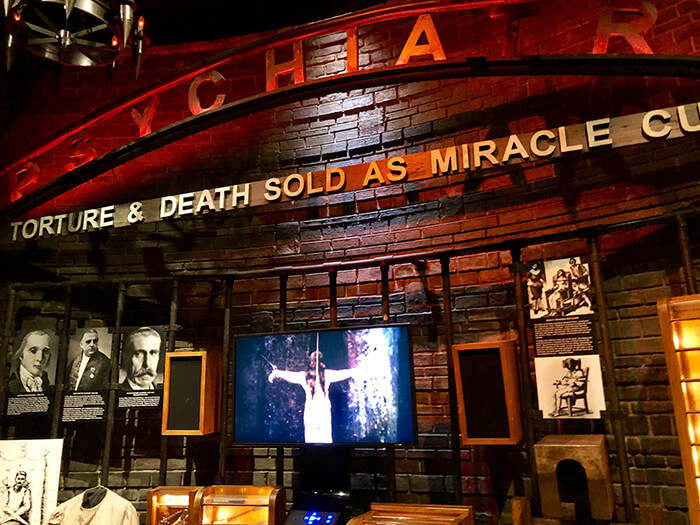
Image: www.busytourist.com
The Controversies: A Closer Look
The criticisms of modern psychiatry are multifaceted and often deeply personal. Here are some key areas that have fueled debates:
- Misdiagnosis and Overdiagnosis: The DSM, as mentioned earlier, has been scrutinized for its potential to misdiagnose or overdiagnose, leading to unnecessary medication and even social stigma. The very act of labeling someone with a mental illness can be stigmatizing and limit their opportunities.
- Over-reliance on Medication: While medications can offer temporary relief, they often fail to address the root causes of mental distress. The focus on medication can sometimes impede the exploration of underlying psychological and social issues.
- Ethical Concerns : The use of powerful psychotropic medications, especially on vulnerable populations like children and the elderly, has raised ethical concerns. There are questions about informed consent, the potential for long-term side effects, and the potential for dependency on drugs.
- The “Chemical Imbalance” Myth: The notion that mental illness is caused by a chemical imbalance in the brain is a common misconception. While neurochemical imbalances can play a role in certain conditions, they are not the sole cause of mental illness.
The Search for Alternatives
The critiques of psychiatry have fueled a growing movement toward alternative approaches to mental healthcare. This movement embraces a holistic view of mental wellbeing, considering the interplay of mind, body, and spirit. Some emerging practices include:
- Integrative Therapies: These approaches combine traditional psychotherapy with complementary practices like yoga, meditation, and nutritional counseling.
- Mindfulness and Compassion Practices: Mindfulness meditation and other compassion-based practices have shown promise in reducing stress, improving emotional regulation, and fostering resilience.
- Existential and Humanistic Therapies: These therapies focus on exploring the meaning and purpose in life, helping individuals develop a sense of personal responsibility and self-acceptance.
- Community-Based Mental Health Services: A growing movement is prioritizing community-based services that offer a more personalized and culturally sensitive approach to mental health care.
Psychiatry: An Industry Of Death Museum
A Call for Critical Evaluation
It’s important to acknowledge that psychiatry has played a vital role in reducing suffering and improving the lives of millions. However, it’s equally crucial to engage in critical evaluation, acknowledging the limitations and controversies surrounding the field. This critical examination, combined with the exploration of alternative approaches, allows us to move towards a more compassionate and effective system of mental health care.
The future of mental health lies in a nuanced approach, one that combines the best of modern medicine with the wisdom of ancient practices and the power of human connection. It’s a future where we treat mental illness not as a disease, but as a natural part of the human experience, and where we empower individuals to make informed choices about their own well-being.



/GettyImages-173599369-58ad68f83df78c345b829dfc.jpg?w=740&resize=740,414&ssl=1)


